Inflammation: The Root of Disease
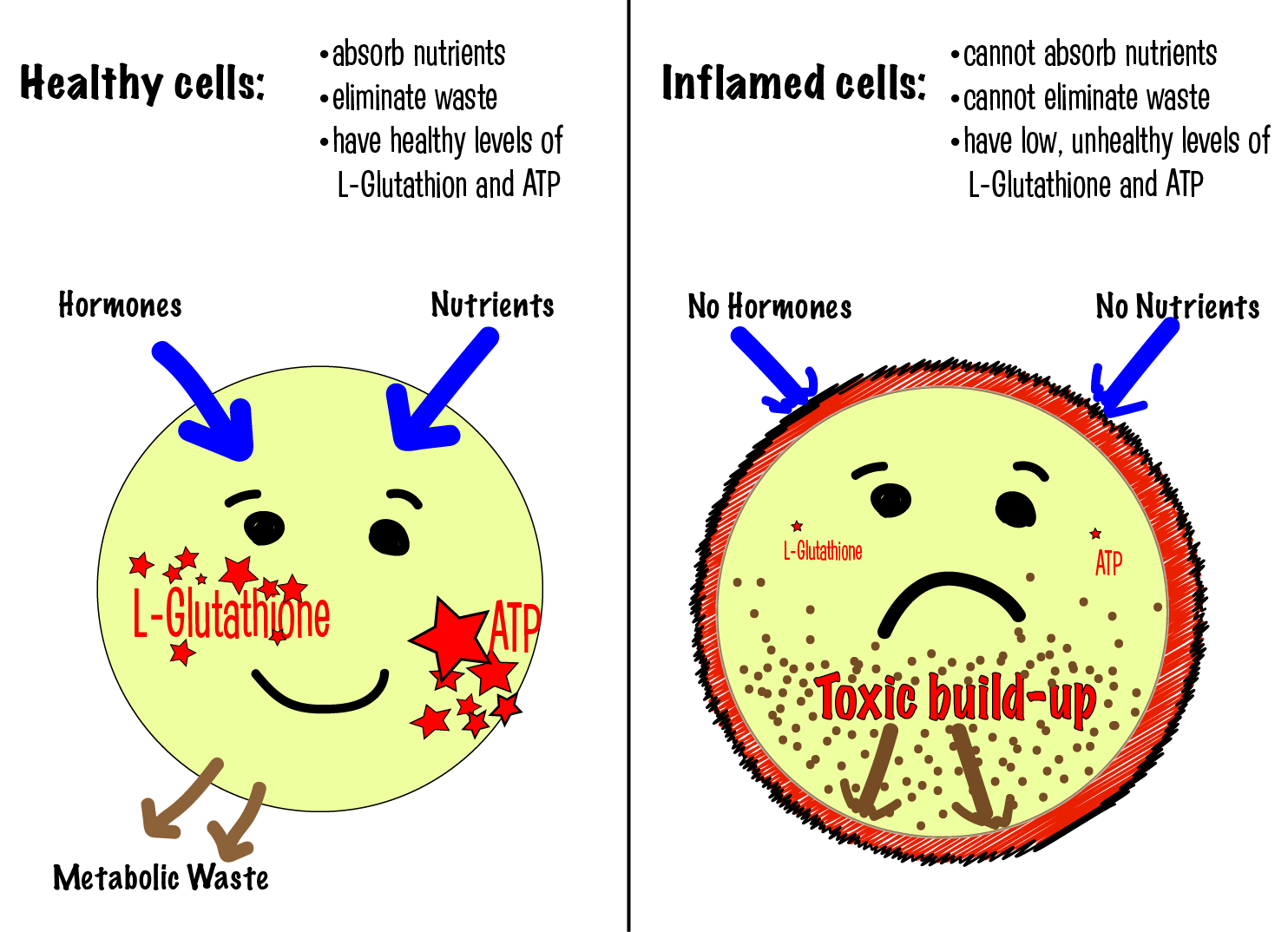
All of our human life happens inside our very tiny human cells. Each cell wall consists of a membrane made of a phospholipid bilayer that functions similarly to soap with a hydrophobic interior and a hydrophilic exterior. The food we eat gives the cells the fuel – in the form of sugars, glucose and fats. We breathe air to give the cells oxygen. The spark – which are the electrical impulses from our nervous system – create the energy we need. Through the membrane, our cells eliminate the burned fuel, metabolic waste, and any harmful substances that have entered the cell through the membrane.
Chronic inflammation is more common than we think.
If our body is using energy to unnecessarily fight a perceived “invasion”, then it has less energy for normal functions. More importantly, with less energy available, our bodies cannot produce anti-inflammatory compounds such as glutathione, one of our bodies’ major antioxidant. In addition, adenosine tri-phosphate (ATP)— the energy molecule used by our cells is being used to fight a threat that isn’t real. At the end of the day, we have less energy and lower levels of antioxidants creating vulnerability for potentially diseased states.
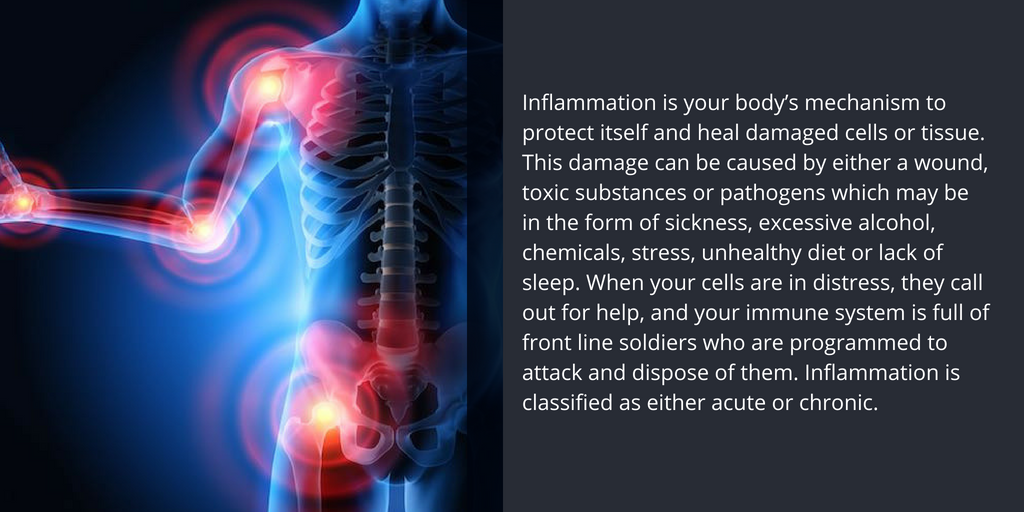
You may not always be able to visually see the effects of inflammation, but there are signs that indicate its presence.
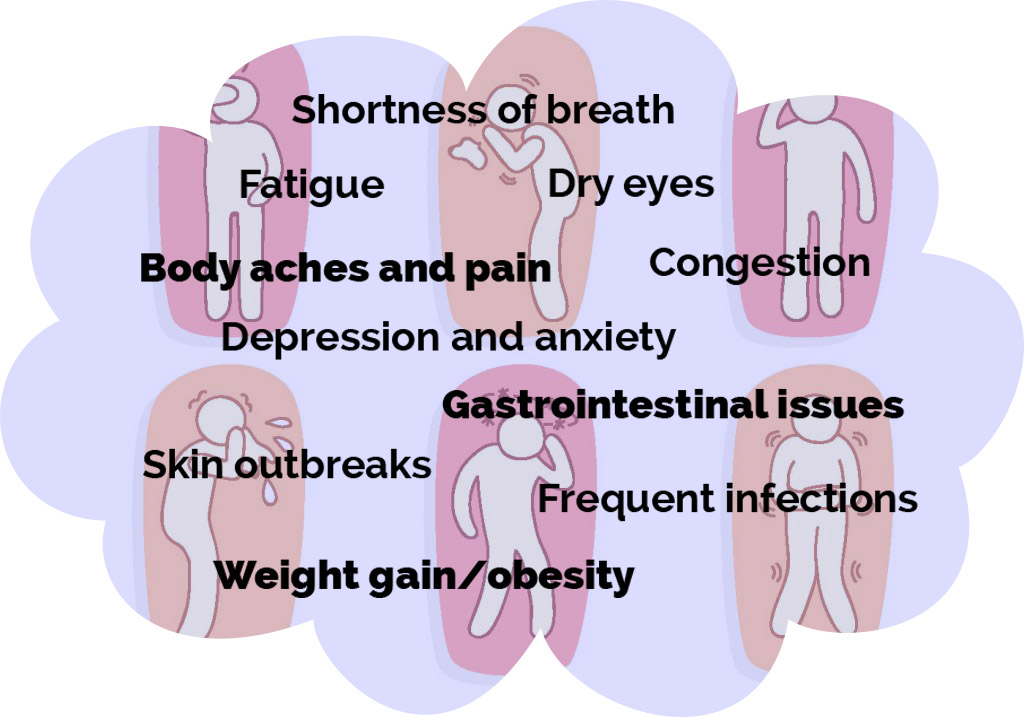
Chronic inflammation can manifest itself in many ways, including digestive issues and skin problems, exhaustion, and recurring infections.
Chronic inflammation is believed to play a role in the development of several long-term illnesses like cancer, heart disease, autoimmune diseases and even brain diseases such as Alzheimer’s and dementia.
Digestive: Since the majority of your immune system is located inside your digestive tract, it is important to keep this healthy. Eating nutrient-dense, whole foods will encourage good digestive enzymes and healthy microbiota and enable your digestive system to process your food and effectively eliminate waste. A poor diet high in many processed foods, including hydrogenated and partially hydrogenated oils, high in sugar and white flour causes your immune system to respond with an inflammatory response to protect its healthy cells. If you have been tested by your doctor and suffer from specific food allergens, like gluten or dairy for example, these foods can also trigger an inflammatory response.
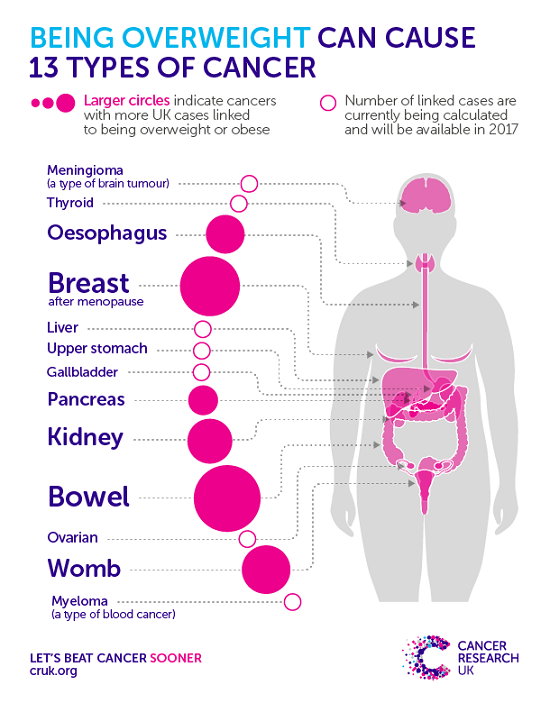
Obesity: Having excess body fat, especially visceral fat around the hips and abdomen, contributes to chronic, low-grade inflammation, which can cause DNA damage and an increase in risk factors for certain types of cancer. According to the National Cancer Institute, obesity is linked to at least 13 different cancers. However, half of all cancer cases could be avoided using the information we already know (i.e. keep a healthy diet, don’t smoke, and get good amounts of sleep and exercise).
Fat tissue will create inflammation that uses up nutrients and makes it more challenging for your body to clear toxic substances. It also switches how cells grow and use energy. Dr. Bongiorno
Toxins: If you are inhaling or ingesting large amounts of toxic substances, they can be stored in fatty tissue and then eventually your healthy cells. While our bodies can handle a certain amount, an overload can cause healthy tissue and cell membranes to become inflamed and damaged. Additionally, processed foods and an unhealthy gut will negatively affect your body’s ability to process exposure to toxic substances. If you are exposing yourself to more toxins than your body is eliminating, this may create inflammation.
Foods to eat include plenty of colorful vegetables and greens, and foods containing healthy fatty acids, such as those found in nuts and avocados. Additionally, drink plenty of clean water so your cells stay hydrated and can perform at their optimal level!
Learn More About Diet: Jennifer Whitney
Dr Rosie Main has nutrition and exercise plans to support your healing
- Regular exercise helps fight inflammation.
Get enough sleep and reduce stress. Poor sleep and stress are known triggers of inflammation. According to a study performed by Emory University and presented at the 2010 American Heart Association Scientific Sessions, getting less than six hours of sleep per night is associated with higher levels of inflammation. This is also linked with an increased risk of heart attack and stroke.
- Reducing stress and getting enough sleep helps fight inflammation.
In addition to lack of sleep, excessive levels of long-term stress can negatively affect your gut and compromise the production of enzymes that aid in the digestive process. For your best performance, it is optimal to get eight hours of sleep each night, with at least five of those hours being continuous or uninterrupted.
Our Local Practitioners All Shared Numerous Ways To Support Your Healing From Inflammation visit their sites to learn more:
David DeHaas of Living Waters Wellness Center
Malisa Williams, LMSW, CMSP of Renew Wellness
Dr. Michael Karlfeldt of The Karlfeldt Center
Tamra Geryk RN of Functional Medicine of Idaho
Dr. Rosie Main DC of Main Health Solutions
Jennifer Whitney of Restoring Nutrition
Lisa Hevern, an Independent DoTerra Wellness Advocate
Dr. Jon Harmon of Clear Mind Idaho
Dr. Andrew Rostenberg of Red Mountain Natural Clinic
Sources:
“Anti-Inflammatory Nutrition Research.” Inflammation Research Foundation, www.inflammationresearchfoundation.org/
“Acute Inflammation.” Washington.Edu. University of Birmingham, n.d. Web. 05 Oct. 2016.
DiCorleto, PhD Paul. “Why You Should Pay Attention to Chronic Inflammation.” Health Essentials from Cleveland Clinic, 25 July 2016, health.clevelandclinic.org/2014/10/why-you-should-pay-attention-to-chronic-inflammation/.
Gushée, Sophia Ruan. A to Z of D-toxing: The Ultimate Guide to Reducing Our Toxic Exposures. N.p.: n.p., n.d. Print.
Heid, Markham. “The Habit That Can Save Your Life.” Prevention. N.p., 16 Aug. 2012. Web. 05 Oct. 2016.
“How being overweight causes cancer.” Cancer Research UK, 6 Apr. 2017, www.cancerresearchuk.org/about-cancer/causes-of-cancer/bodyweight-and-cancer/how-being-overweight-causes-cancer.
Hume, Tim, and Jen Christensen. “WHO: Imminent Global Cancer ‘disaster’ Reflects Aging, Lifestyle Factors.” CNN. Cable News Network, 04 Feb. 2016. Web. 05 Oct. 2016.
Nordqvist, Christian. “Pain / Anesthetics Bones / Orthopedics Immune System / Vaccines Arthritis / Rheumatology Inflammation: Chronic and Acute.”Medical News Today. MediLexicon International, 16 Sept. 2015. Web. 05 Oct. 2016.
Paddock, Catharine. “Cardiovascular / Cardiology Sleep / Sleep Disorders / Insomnia Heart Disease Stroke Poor Sleep Tied To Inflammation, A Risk Factor For Heart Disease, Stroke.” Medical News Today. MediLexicon International, 15 Nov. 2010. Web. 05 Oct. 2016.
Pevzner, Holly. “10 Ways to Reduce Inflammation.” EatingWell. Eating Well Magazine, June 2012. Web. 05 Oct. 2016.
Rattue, Grace. “Immune System / Vaccines How Does The Immune System Power Inflammation?” Medical News Today. MediLexicon International, 05 July 2012. Web. 05 Oct. 2016.
Samadi, David. “Inflammation: The Battle to the Death Inside Our Bodies.” The Observer. N.p., 11 Sept. 2015. Web. 05 Oct. 2016.